Diagnostics and therapy of prostate cancer with PSMA radioligands
[03.05.2017] The introduction of peptide-based small radioligands targeting the prostate specific membrane antigen (PSMA) has had a tremendous impact on the diagnosis and treatment of prostate cancer (PCa) in recent years.
PSMA is a cellular surface molecule that is frequently highly overexpressed in prostate cancer, especially in aggressive tumors with a high Gleason score. Thus it presents an ideal target for highly specific and sensitive imaging and therapy in prostate cancer.
PSMA-based imaging is used for staging in case of suspected aggressive tumors (intermediate and high-risk cases, i.e. PSA > 10 ng/ml, clinical stage T2b or higher or a Gleason score of 7 or larger) in order to exclude occult metastasis and select the optimal treatment strategy prior to curative surgery or radiotherapy.
Moreover, the precise diagnostic information delivered by modern PET/CT with PSMA radioligands permits a more accurate detection of tumor recurrence in case of suspected biochemical relapse, allowing accurate pin pointing of tumor lesions for site directed therapy (i.e. surgery or radiotherapy) (Figure 1).

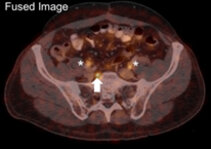
Figure 1:
PSMA-PET/CT showing of a lymph-node recurrence (arrows) in a patient with a PSA-level of 0.2 ng/ml. Note the strong PET-signal in the unsuspecting, regular-sized lymph node on CT. *=ureter.
In addition to these novel imaging approaches PSMA-ligands can also be labelled with therapeutic radionuclides (e.g. the beta-emitter Lutetium-177) in order to selectively treat advanced disease. This promising therapy has been introduced at our department in 2015. The therapy is usually well tolerated and only rarely leads to transient hematological impairment (e.g. in patients with prior chemotherapy).
Due to the strong over-expression of PSMA in many tumor cells, it is possible to achieve high radation doses even in highly chemo- or hormone-therapy resistant tumors and impressive responses to therapy (Figure 2) have been achieved even in patients without any other therapeutic options. In contrast to the ambulatory PET/CT-examination, PSMA-radioligand therapy is performed on ward in order to adequately monitor the patient, to perform intratherapeutical dosimetry and to comply to the radiation protection legislation.

Figure 2:
Three-dimensional maximum intensity projections (MIP) of a PSMA-PET/CT scan of a patient with advanced prostate cancer. The first scan (A) shows multiple osseous and lymphonodular metastases at a PSA-level of 10.8 ng/ml. One year later (B), after three cycles of PSMA radioligand therapy, the patient presents with a complete remission at a PSA-levewl of 0.05 ng/ml.
Thus, the theranostic approach with PSMA radioligands opens up new and promising possibilities for both highly specific and sensitive imaging and, consecutively, therapy of prostatic cancer.