Radiation Oncology
Modern radiotherapy treatment – effective and gentle

What is radiotherapy? How will I be treated? What effects or side-effects will the treatment have? These and other questions preoccupy patients who have to undergo radiotherapy treatment.
My colleagues, staff and I are particularly concerned with explaining the procedures prior to, during and after radiotherapy treatment in a detailed personal discussion: not only to our patients and their relatives, but also to colleagues from other medical specialities. If you have questions or problems, please raise them with us.
It is very important to all members of the radiotherapy team (radiation oncologist, medical physicist radiographers and nursing staff) that not only do our patients receive the best medical care, but also that they and their relatives our full attention. The tasks of a university clinic are to provide excellent patient care, to push the scientific boundaries and pass on knowledge. To this end the philosophy of our clinic is based on three pillars: patient care, research and teaching. On the following pages you can find information relating to these three areas whether you are a patient, relative, physician, scientist or student.
Welcome to the Department of Radiation Oncology,
University Medical Center Freiburg!
Yours,
Univ. Prof. Dr. med. Anca-L. Grosu
Chair of Department of Radiation Oncology
Medical director of ambulatory health care centre of University Medical Center Freiburg
Treatment

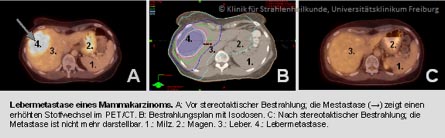
Stereotactic radiotherapy is a very precise form of image guided radiotherapy (IGRT) where strictly defined target volumes – benign and malignant tumors – are treated with high radiation doses. To achieve a precision within 1 millimeter, the body part in question has to be positioned and fixated very carefully. A steep dose gradient to the surrounding normal tissue guarantees optimal protection of healthy cells. The radiation dose is applied in 1 to 10 therapy sessions (fractions).
The term radiosurgery is used when only one fraction is applied. Similar to actual surgery, the tumor is treated in one single day.
Stereotactic radiotherapy / radiosurgery is most commonly used in cases of brain tumors, but in recent years its application in tumors of the lung, liver, kidneys and metastases of the bone has become indispensable.
The Department of Radiation Oncology, University Medical Center Freiburg is among the leading radiation centers on a national and international level in the use of this method. We utilize Varian TrueBeam STX Novalis Radiosurgery equipment, which is specially adapted to the requirements of stereotactic radiation.
Moreover, we initiate and participate in national and international clinical trials to develop new and innovative treatment regimens.
Intensity modulated radiotherapy (IMRT) is especially suitable for tumors with a complex 3-dimensional morphology located in the vicinity of radiosensitive organs. Multiple radiation fields coming from different directions and with individually modulated intensities converge in the tumor (target volume) forming “dose topographies”. The overlap of all these dose structures results in an even dose distribution in the complex shape of the target volume, while carefully protecting the adjacent radiosensitive organs. The modulation of the intensity of each individual radiation field is achieved by the movable and automatically controlled leaves of the multi-leaf collimator (MLC) within the accelerator. With the aid of powerful computers the expert team of medical physicists determines the highly complex sequence needed for each patient and treatment plan, which is then validated by extensive measurements at the linear accelerator.
Image Guided Radiotherapy (IGRT) combines imaging and radiotherapy in the same irradiation unit. This allows the reproducible and precise positioning of patient and target volume at the beginning and during the radiation treatment. At the same time 3-dimensional imaging permits the radiotherapist to react immediately to anatomical changes of patient and tumor.
Here at the Medical Center – University of Freiburg we perform intraoperative radiotherapy (IORT) either with the mobile Intrabeam system by Carl Zeiss AG or with the Mobetron linear accelerator by MD51, directly in the operating room.
During IORT the radiotherapist, the surgeon and the medical physicist work very closely together. In contrast to other radiation methods, healthy organs can be moved out of the radiation beam and intraoperative findings can directly influence the extent of the radiotherapy.
The Intrabeam system generates low energy X-rays, which are most effective at close range. With a spherical applicator the tumor bed, or resection cavity, can be directly irradiated.
The Mobetron system is a mobile linear accelerator using electron radiation. This provides careful control of radiation penetration depth, helping to protect healthy organs. The mobility of the device is suitable for adapting radiation to the individual case.
These specialized mobile units enable us to provide optimum protection of healthy tissue. The devices can be utilized for a wide range of surgical interventions, e.g. in senology (breast cancer), gynecology, and urology, as well as abdominal, plastic and thoracic surgery.

Intraoperative Radiotherapy in Breast Cancer
- New treatment improves chances of recovery
- Optimal protection of healthy tissue
- Shorter duration of treatment
Breast cancer is the most common form of cancer in women. In recent years, a new breast-conserving treatment has gained importance: intraoperative radiotherapy (IORT). The Department of Gynecology and Obstetrics of the University Medical Center Freiburg (Director Prof. Dr. Dr. h. c. G. Gitsch) together with the Department of Radiation Oncology (Director Prof. Dr. med. A.L. Grosu) implement this innovative and beneficial method with the Intrabeam radiotherapy system built by Carl Zeiss AG, Germany. Prof. Dr. Anca-Ligia Grosu emphasizes the high radiation dose that can be applied directly in the tumor region with IORT. The radiotherapist and the surgeon collaborate closely during the procedure. According to Dr. T. Erbes, Head of the Senology Unit of the Department of Gynecology and Obstetrics, IORT offers a very precise way to treat the tumor bed, where there is the greatest risk of cancer recurrence, while still in surgery. The soft X-rays are most effective at close range. Thus adjacent organs, which are beyond the radiation field, can be protected from exposure to radiation while still maintaining a high radiation dose in the tumor bed.
Last but not least, the combination of IORT and conventional radiotherapy of the whole breast results in a much shorter duration of treatment.
Brachytherapy is a form of radiotherapy where a sealed radiation source is placed inside or next to the area requiring treatment.
In certain cases the artificial overheating of tumors by electromagnetic waves (interstitial hyperthermia) can enhance the effect of radiotherapy and chemotherapy.

Since 2016, the Department of Radiation Oncology of the Medical Center – University of Freiburg offers treatment with modern tomotherapy technology. The installation of the tomotherapy system is the first of its kind in the region. The equipment is a combination of a high resolution computer tomography scanner and a linear accelerator. An X-ray is spiralling around the patient, who is placed in a horizontal position. In this way, 3-dimensional images are generated, as in a CT scan, which allow the exact localization of the tumors. At the same time radiotherapy is applied in a highly conformal manner, i.e. precisely matched to the target area. This new method offers a better dose distribution and protection of healthy tissue than traditional radiation technologies, especially in cases of extensive and/or multiple tumors.
Since December 2023, the Department of Radiation Oncology, Medical Center - University of Freiburg, offers the possibility to continuously adapt the treatment to the daily changes in the patient's body (online adaptive radiotherapy, oART).
The goal of online adaptive radiotherapy is to adapt the patient's treatment plan to the current anatomy in order to account for differences due to organ movement and organ filling between fractions prior to daily treatment. This is made possible by the latest generation of linear accelerators – Ethos with the integrated online 3D imaging system HyperSightTM by Varian Medical Systems. HyperSightTM is the fastest CBCT imaging available and provides the best image quality for oART.
Radiotherapy (Radiation oncology/Radiation therapy) is concerned with the medical application of ionising radiation. The aim of which is to treat disease - in particular malignant but also benign - , to delay its progression or relieve discomfort. In addition to surgery and medication, radiotherapy plays an important role in the treatment of cancer. In this respect it may be employed alone, prior to, during or after surgery.
Moreover it is possible to combine radiotherapy with tumouricidal pharmaceuticals (chemotherapy). It is possible to administer a chemotherapy or immunotherapy pharmaceutical that increases the tumour's sensitivity to radiation. To better protect healthy tissue radio-protective substances can also be administered. The correct treatment combination is dependent on the case and is defined in an individual treatment concept specific to the patient. Depending on the type of cancer radiotherapy is used in either a curative or palliative setting. In the case of a curative therapy the aim is to completely destroy the tumour. If this can be achieved then the patient is cured. It can also be sensible to preventatively irradiate after surgery, in order to destroy malignant cells which may remain at the surgical site. If cure of a particular cancer is no longer possible, for example if it has already metastasized, palliative radiotherapy is employed to relieve, or even eradicate, symptoms such as pain, shortness of breath, bleeding and paralysis. The well-being and quality of life of the patient would, thereby, be greatly improved.
Mode of operation
Radiotherapy uses radiation to transmit energy that will disrupt the growth of cells in the irradiated tissue. More precisely: Radiation therapy damages the genetic material (DNA) within the cell nucleus, thereby inhibiting cell division. While healthy cells can repair the damages, tumor cells are less adaptive: They are stopped in their growth, or even destroyed.
The required dose of radiation – measured in “Gray” (Gy), an international unit named after physicist Louis Harold Gray – depends on the radiation sensitivity and the position of the tumor. The treatment plan determines for each individual patient the dosage and fractionation, i.e. the number of “single portions” for delivering the required dose. The plan must also consider the possible irradiation of healthy tissue and organs encountered by the radiation beam on its way to the tumor.
Usually the total dose is divided into several radiation sessions, or fractions. Typically fractions of 1.8 to 2.0 Gy are applied. Healthy cells need a certain amount of time to recover from radiation effects. If the next fraction is delivered after completion of this “repair work”, the patient tolerates the treatment better and has fewer side effects. Therefore radiotherapy may stretch over several weeks.
Special situations, however, in particular with high-precision radiotherapy, may provide indication of higher single doses up to 20 Gy. This is possible when such a small amount of healthy tissue is irradiated that – as in surgery – “scarring” of the affected area becomes acceptable.
Our equipment
| Linear accelerators | ||
| 1x Synergy | Elekta | IMRT/VMAT/IGRT |
| 2x TrueBeam STx with ExacTrac | Varian, BrainLab | SRS/IMRT/VMAT/IGRT |
| 1x Varian ETHOS with HyperSightTM | IMRT/VMAT/IGRT/oART | |
| 1x Tomo | Accuray | IMRT/IGRT |
| 1x Mobetron | IntraOp | IOERT |
| 1x IntraBeam | Zeiss | IORT |
| Brachytherapy and Hyperthermia | ||
| 2x HDR Afterloaders | Elekta | Microselectron-HDR |
| Thermography-controlled wIRA-Hyperthermia | Heckel Medizintechnik GmbH | Hydrosun TWH1500 |
| Imaging | ||
| 1x CT - Simulator | Philips | |
| 7x 3D-Surface Image Guidance | C-RAD | |
| Interventional/Brachytherapy Imaging | MedPhoton | ImagingRing |
| BK Medical | bk5000 Premium | |
Planning and implementation of radiotherapy

A typical radiotherapy treatment, performed at a linear accelerator (linac), comprises the following steps:
1. Definition of the treatment concept
An individual treatment concept is determined for every patient within the so called tumour conference, at which specialists from different medical disciplines participate: Surgeons, internists, pathologists, radiologists, psycho-oncologists, nuclear medicine physicians and palliative medicine physicians.
History
The Beginnings of Radiotherapy
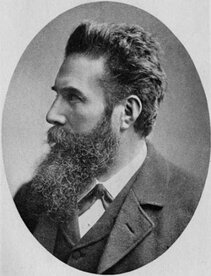
On 8 November 1895, physicist Wilhelm Conrad Röntgen made a revolutionary discovery at the Institute of Physics of the University of Würzburg: a new kind of radiation, which he called X-rays. They made it possible to glance inside the body, thus opening up entirely new diagnostic possibilities. It was only two weeks later that the first Roentgen image in history was taken: after an exposure time of 20 minutes, the bones of his wife’s hand were displayed.
Statistics

- Intensity modulated radiotherapy (IMRT) = 22.943 procedures per year
- Stereotactic radiotherapy = 752 procedures per year
- Intraoperative radiotherapy (IORT) = 86 procedures per year
Awards
- Prof. Dr. med. Anca-L. Grosu is Honorary Fellow of the American College of Radiology (ACR), Washington DC
- Prof. Dr. med. Anca-L. Grosu receives Alfred Breit Prize 2020 from the German Society for Radiation Oncology. Read more...
- Prof. Dr. Dimos Baltas appointed President of the German Society for Medical Physics. Read more…
- PD Dr. Constantinos Zamboglou receives Hermann Holthusen Prize from the German Society for Radiation Oncology Read more…
- Prof. Dr. med. Anca-L. Grosu, MD elected as member of the prestigious German National Academy of Sciences “Leopoldina” Read more...