Prostate cancer
Prostate cancer: Description
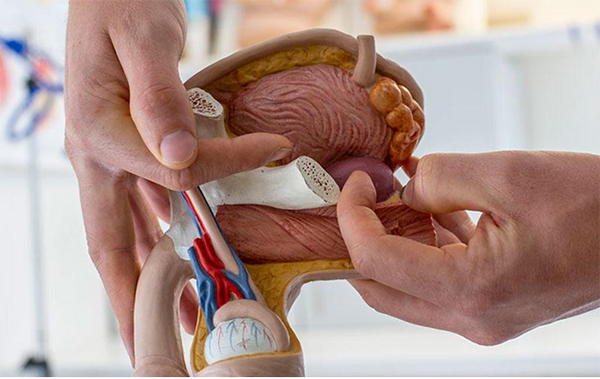
Prostate cancer is a malignant tumor of the prostate gland. The prostate gland lies under the bladder and produces a secretion that is part of the seminal fluid. Below the prostate is the rectum: this localization allows palpation and assessment of the prostate through the rectum. The functions and growth of the prostate are affected by the sex hormone testosterone.
Prostate cancer is the most common form of cancer in men, and with early detection and optimal treatment has a relatively good prognosis. The mean age of onset is approximately 69 years.
Prostate cancer: Symptoms
In its early stages, prostate cancer is in most cases asymptomatic. At an advanced stage it may interfere with urination (micturition). Then patients complain of pollakisuria (frequent urination), dysuria (burning sensation), nocturia (urination at night) or alguria (pain). Other possible symptoms of the advanced disease stage are prolonged urination with a weak urinary stream, a buildup of residual urine or erectile dysfunction.
If metastasis has already occurred, there may be symptoms directly linked to the metastases, even if the primary tumor remains asymptomatic. Very often, there are sometimes severe pains in the area of each bone metastasis, however only rarely does blood admixture in the urine (hematuria) or ejaculate (hematospermia) occur. Bone metastases can lead to pathological fractures or neurological impairment, and metastases in the lymph nodes can cause edema (excess fluid) in the legs and scrotum.
Prostate cancer: Causes and Risks
The causes of the disease are so far largely unknown, but patients with a genetic predisposition (a cluster of disease cases in the family history) are definitely in the risk group. This is especially true if the patient's father was diagnosed with prostate cancer at under 60 years of age. Obesity, a high fat diet (especially animal fat) and lack of physical activity appear to increase the risk of later developing prostate cancer.
Prostate cancer: Examination and Diagnosis
Diagnosis of prostate cancer can take place using various examination methods. During a digital rectal examination (DRE), palpation may already lead to a diagnosis of suspected prostate cancer. The most important test is determining the level of prostate specific antigen (PSA) in the blood. This level constantly increases, higher and faster, in almost all prostate cancers. But PSA is not specific to prostate cancer, meaning that raised levels can also occur with a significantly enlarged benign prostate (benign prostatic hyperplasia or BPH) or with inflammation of the prostate (prostatitis). When in doubt, a transrectal ultrasound guided prostate biopsy should be performed, in which at least 12 tissue samples are usually taken from the prostate. While ultrasound from outside through the full bladder can only accurately determine the size of the prostate, with transrectal ultrasound (TRUS) the internal structure of the prostate can be precisely assessed, and in some cases the tumor can even be displayed. Today, magnetic resonance imaging (MRI) is used for evaluation of the local tumor stage. In case of a primarily negative biopsy accompanied by a rising PSA level, fusion-based guided biopsy techniques can be applied. Here, the images from a previously conducted MRI or PET-CT examination are imported into the current ultrasound image, so that one can see the exact points where biopsies should be taken. The biopsy is performed through the perineal area and under anesthesia.
Histopathological examination of biopsies is the central part of the diagnosis. Aside from the type of prostate cancer, the Gleason score should also be specified. This value indicates the growth pattern and aggressiveness of the prostate cancer.
In case of a confirmed cancer diagnosis, an accurate staging of the tumor (e.g. using the TNM classification) is required, and further tests - abdomen sonography, computed tomography (CT), magnetic resonance imaging (MRI), whole-body bone scintigraphy or PSMA (prostate specific membrane antigen)-PET CT examination is necessary in order to exclude metastases or for localization.
Prostate cancer: Treatment
The core methods for treatment of prostate cancer are surgery, radiation therapy and drug therapy (hormonal therapy and/or chemotherapy). In case of localized prostate cancer, a radical prostatectomy (RPE) is usually carried out. In this surgery the prostate, seminal vesicles and regional lymph nodes are removed. The operation is categorized according to the following ways in which it may be carried out: retropubic radical prostatectomy (RRP), radical perineal prostatectomy (RPP), laparoscopic prostatectomy (LRP) or robot-assisted laparoscopic prostatectomy (RALP).
Radiotherapy offers an alternative to surgery in case of localized prostate cancer. A distinction must be made here between percutaneous radiotherapy (with linear accelerator) and brachytherapy: low-dose-rate brachytherapy (LDR) and high-dose-rate brachytherapy (HDR). In LDR, exclusively small radiation particles (seeds) are introduced into the prostate, which continue radiating freely from inside. In HDR, in addition to the seeds, irradiation is also performed from the outside (combined interstitial and percutaneous radiotherapy).
Because the prostate is a hormone-dependent organ, antihormonal therapy is often used in men with advanced prostate cancer. In this case, either the production of testosterone is suppressed (normally by hormone injections) or the binding site for testosterone on the tumor cells is blocked (usually by antiandrogens in tablet form). All types of hormone therapy have side effects and can only delay the disease progression. Sometimes hormone therapy is used concomitantly with radiotherapy, as this can enhance the effects on the tumor cells. Chemotherapy is used in patients with metastatic prostate cancer as a palliative treatment measure.

Prostate cancer: Course and Prognosis
A complete cure is possible if the tumor has been completely removed surgically, or else irradiated with curative intent, in which case the prognosis for long-term survival is 80-90 percent. However, this is only possible if the tumor was discovered early. In case of advanced metastatic prostate cancer, the prognosis is much worse. Through the use of all of today's modern treatment options, the long-term course can also be stabilized in many cases. But a cure is unfortunately not yet possible for these patients.
The strategy of "active observation" (active surveillance or AS) is aimed at supervision and checkups, and is based on individual criteria (patient age, risk of disease progression, PSA level, Gleason score, number of positive biopsies etc.) and the desires of the patient. There is at first no active treatment, but only an examination and check of PSA levels every three months, with a repeat prostate biopsy planned after 12-18 months. This form of therapy is so far recommended only for low risk prostate cancer.
Prostate cancer: Miscellaneous/Other Comments
The Prostate Center in the Department of Urology at the Medical Center - University of Freiburg is the contact point for all patients with prostate disease. Comprehensive information about the patient is the basis for individual and holistic diagnosis and treatment. The clinic offers every kind of diagnostic and therapeutic procedure in order to enable optimal patient care. The Prostate Center involves a range of disciplines such as urology, radiotherapy, oncology, radiology, nuclear medicine and pathology. The treatment of tumor diseases is carried out according to international guidelines and in close cooperation with the Comprehensive Cancer Center Freiburg (CCCF).