Is it possible to find out if I am at risk of Alzheimer’s disease?

Prof. Dr.Dr.T. Meyer © UKF
[16.10.2025]
In an interview with Professor Dr. Dr. Philipp T. Meyer, Medical Director of the Department of Nuclear Medicine at the Medical Center – University of Freiburg, we explore how PET is used in the diagnosis, prognosis and treatment of memory disorders, which PET tracers provide the most informative results, and the opportunities and limitations of this method. This interview takes place against the background of the approval and application of the first causal Alzheimer's therapy in Germany.
In which cases do you recommend using PET for patients with cognitive disorders?
PET scans are more accurate for diagnosing and predicting outcomes than clinical exams or imaging methods like CT or MRI. PET is often used for people with dementia or in its prodromal stage, called mild cognitive impairment (MCI). Its main purpose is to detect or rule out neurodegenerative brain diseases such as Alzheimer’s disease.
A PET scan is especially recommended when the cause of memory or – more general – cognitive problems is still unclear after other possible (and reversible) causes have been excluded and additional tests, such as a spinal fluid test, have been done.
It’s also important that the PET scan results have relevant consequences for the patient. This doesn’t only mean starting a specific treatment (such as for Alzheimer’s disease) — it can also mean avoiding unnecessary or harmful treatments, giving a more accurate prognosis, and helping patients and their families plan and make informed decisions about care and daily life.
What are the differences between FDG PET, amyloid PET, and tau PET, and how early can a PET provide reliable indications of Alzheimer's or other forms of dementia?
One important tool is the amyloid PET scan. This test can detect the characteristic protein deposits in the brain — called amyloid plaques — that are associated with Alzheimer’s disease. Remarkably, these changes can sometimes be seen 20–30 years before dementia symptoms appear, at a time when people are still cognitively intact, fully active and independent. In everyday medical practice, amyloid PET is typically used once some mild symptoms are present. If these are due to Alzheimer’s disease, the scan often shows clear and advanced signs of amyloid buildup.
Another important scan is the tau PET, which visualizes tau deposits, a second key change seen in Alzheimer’s disease. Early on, tau PET results may show only minor abnormalities, but as the disease progresses, tau spreads more widely through the brain. Tracking this progression helps doctors determine the biological stage of Alzheimer’s disease. Understanding these changes is not only helpful for diagnosis but also increasingly important for prognosis as new treatments become available — for instance in therapies that target amyloid plaques especially in the early stages of the Alzheimer’s disease.
FDG PET is a method that measures how the brain uses glucose, which reflects its activity and function. FDG stands for fluorodeoxyglucose. Unlike amyloid and tau PET scans, which are mainly used to diagnose Alzheimer’s disease, FDG PET is more universal — it can detect abnormal metabolic patterns in many different neurodegenerative diseases. This includes not only dementia but also Parkinson’s disease and related syndromes. In everyday clinical use, FDG PET can already show disease-specific metabolic changes in most patients at the early stage of mild cognitive impairment (MCI). The patterns seen on FDG PET closely match the type and severity of a patient’s symptoms. This allows for a very accurate diagnosis for most neurodegenerative diseases and to give a reliable prognosis.
Which types of dementia can be distinguished particularly well from one another using PET?
According to new guidelines, amyloid PET is considered the reference method for diagnosing Alzheimer’s disease in a living patient. However, having biomarker-defined Alzheimer’s disease does not automatically mean a person has memory problems or dementia yet. In these cases, tau PET is very useful because it helps determine the biological stage of the disease. This is important because amyloid deposits in the brain can appear decades before any noticeable cognitive problems. In fact, amyloid deposits become more common with age — by age 50, they start to appear in some healthy people, and by age 80, about 40% of cognitively healthy individuals have amyloid in their brains. Current research suggests that Alzheimer’s-related cognitive problems usually only develop when tau deposits are also present in the cerebral cortex.
Amyloid PET can show whether Alzheimer’s disease is present, even if the person has no symptoms yet. If the test is negative, it makes it very unlikely that the person will develop Alzheimer’s in the near future. Tau PET is more precise in showing whether current symptoms are actually caused by Alzheimer’s disease and whether the disease is likely to progress. If amyloid and tau PET scans are normal, or if the symptoms point to a different condition — such as frontotemporal dementia, Lewy body dementia, or cognitive problems related to depression — then FDG PET can be very useful for making the correct early diagnosis.
Are there typical patterns that you can immediately recognize in everyday life?
Yes, the patterns or topography of the findings are usually very characteristic and usually allow for a visual diagnosis. The patterns result from the typical, disease-specific spread of pathological changes in the brain and thus also cause the disease-specific symptoms or deficits.
This is also a major advantage over cerebrospinal fluid examinations: while these often only provide binary (positive or negative) results, PET images show the distribution and severity of the findings. This is very important for assessing whether the patient's symptoms are actually caused by the disease or pathology detected in the cerebrospinal fluid.
What role does PET play in comparison to MRI, cerebrospinal fluid diagnostics, and neuropsychological tests?
Clinical examination, including neuropsychological testing, is the basis of any diagnosis and is indispensable. It determines whether there is any relevant change in cognition, how pronounced it is, and gives a good first impression of what disease could be the cause. Morphological cross-sectional imaging, preferably using MRI, is also essential. It can provide further clues to the underlying disease causing the symptoms and, above all, reveal treatable or non-neurodegenerative causes of cognitive disorders.
Cerebrospinal fluid diagnostics are also often routinely supplemented to rule out other causes like inflammation of the brain and to collect so-called biomarkers of Alzheimer's disease, namely biomarkers of amyloid and tau. However, this already shows that PET examinations are necessary in three scenarios in particular:
- When cerebrospinal fluid testing is not possible or provides borderline or contradictory results.
- When the initial suspicion is already that a patient suffers from a type of dementia other than Alzheimer's dementia. There are no established biomarkers for these diseases in cerebrospinal fluid, whereas FDG-PET can show disease-specific findings.
- When there is doubt as to whether the reported symptoms are actually related to abnormal amyloid findings in the cerebrospinal fluid.
In the context of the novel drug therapies for Alzheimer's disease, amyloid and tau PET are used very effectively to optimally guide the therapy, that is to select the patients who will benefit most and, if necessary, to terminate the therapy once the existing amyloid deposits have been successfully removed from the brain.
Which new tracers or technical developments do you consider particularly promising?
There are currently many promising developments in the field of nuclear medicine or molecular imaging of the brain, especially in cognitive disorders. On the one hand, this concerns dedicated brain scanners that deliver significantly better images in less time and are also much more comfortable for the patient. On the other hand, the probes we inject to measure amyloid and tau deposits provide better contrast and more accurate diagnostics with each new generation. Numerous new probes are also in development that will allow us to visualize fundamental disease processes such as inflammatory changes or other pathologies beyond Alzheimer's disease. At the Medical Center - University of Freiburg, we are in the unique position of being able to draw on all of these techniques.
What role does artificial intelligence play in image evaluation?
We use AI and deep learning in two main ways: on the one hand, these systems support us in our diagnoses, and on the other hand, these techniques improve the image acquisition. The latter allows us to perform very quick examinations lasting only a few minutes and to use only a very low dose of our probes. The radiation exposure of the PET examination is becoming virtually negligible.
How do you think the role of PET in dementia diagnostics will change over the next 5 to 10 years?
I firmly believe that PET will play an essential role in the development, application, and management of new therapies. Innovative probes and therapeutic approaches will also make other neurodegenerative diseases beyond Alzheimer's, which is currently the main focus, accessible for diagnosis and therapy. Ultimately, the above-mentioned techniques will make PET much more widely available. We are living in very exciting times, and experience in recent years shows that there will certainly be other groundbreaking developments that we cannot even foresee at this point.
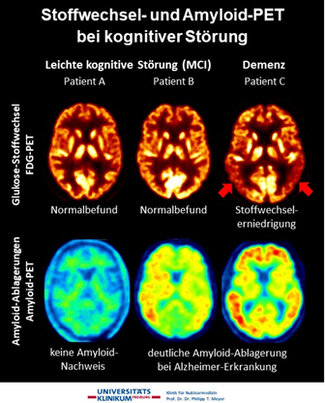
FDG and Amyloid PET in Cognitive Impairment
- Patient A (MCI): Normal metabolism, no amyloid — MCI not due to Alzheimer’s
- Patient B (MCI): Normal metabolism, amyloid present — early Alzheimer’s.
- Patient C (Dementia): Reduced metabolism, amyloid present — advanced Alzheimer’s.
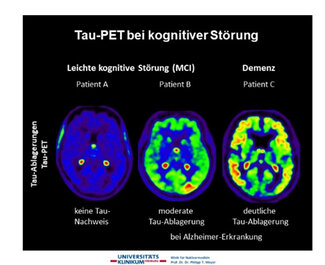
Tau PET in Cognitive Impairment
- Patient A (MCI): No tau deposits
- Patient B (MCI): Moderate tau deposits — early Alzheimer’s.
- Patient C (Dementia): High tau deposits — advanced Alzheimer’s.
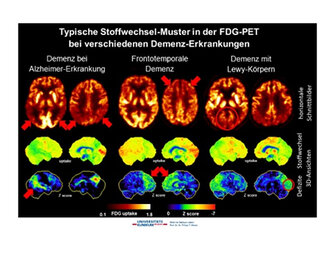
Typical FDG PET Metabolic Patterns in Dementia
- Alzheimer’s Disease: Reduced glucose metabolism in temporal and parietal lobes.
- Frontotemporal Dementia: Decreased metabolism in frontal and temporal lobes.
- Dementia with Lewy Bodies: Similar to Alzheimer’s but also involves the visual cortex.
Notes:
- Top row: Horizontal slices showing FDG uptake (glucose metabolism).
- Middle row: 3D views of uptake (hot-metal scale: black = low, white = high).
- Bottom row: 3D views of metabolic deficits (rainbow scale: 0/black = normal, -7/red = strong deficit).
These patterns help distinguish the three main types of neurodegenerative dementia.