Hernia surgery (groin and abdominal wall hernias)
What is a hernia?
A hernia is a defect in the abdominal wall with protrusion of intraabdominal tissues. Hernias usually have a hernia sac, which consists of peritoneum protruding to the subcutaneous tissue through the defect of the abdominal wall, also called hernia orifice. The contents of the hernia can be different abdominal components e.g. intestinal loops or other intraabdominal tissue as the greater omentum. The surgical treatment of abdominal hernias – especially of groin hernias – is one of the most frequently performed surgical interventions in Germany.
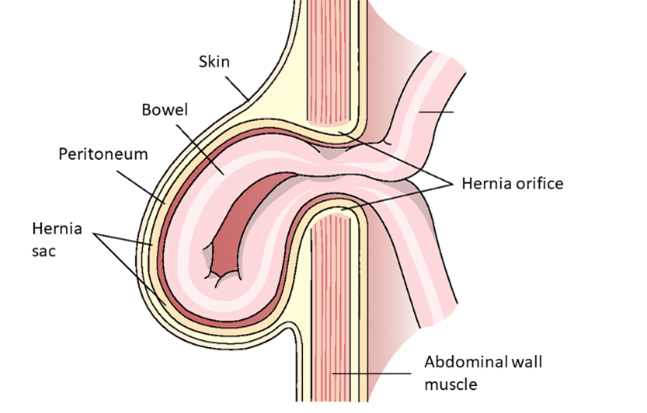
Fig.: Schematic composition of a hernia (with kind permission of Thieme Compliance)
How does a hernia develop?
A hernia develops, if the abdominal wall cannot resist the intraabdominal pressure anymore. This can be due to an inherent weakness of the abdominal wall (groin hernia, umbilical hernia) or an acquired weakness, usually following prior abdominal surgery (incisional hernia). The risk for the development of an incisional hernia following a median laparotomy is between 10-20%. Therefore, incisional hernias are a common problem after general/visceral surgical procedures.
Hernias can occur at all locations within the abdominal wall. However, the most frequent location are in the groin region (groin hernia), at or above the umbilicus (umbilical hernia/epigastric hernia), and at the site of prior incisions (incisional hernia).
What are the symptoms of a hernia?
The two main symptoms of hernias are pain within the affected region and – in most cases - a palpable (and often visible) protrusion of the hernia. This protrusion often disappears spontaneously in the supine position. A hernia orifice can be palpated in most cases as a defect within the abdominal wall.
A major risk consists of the possibility of incarceration of the hernia. An incarceration is characterized by acute and severe pain at the hernia site. In the situation of an incarcerated hernia, the hernia content can no longer be pushed back into abdominal cavity. An incarcerated hernia is a medical emergency and requires immediate treatment to avoid possible life threatening complications.

Fig.: Synthetic mesh used in groin hernia surgery
Which are the therapeutic options?
In many cases, the best treatment of a hernia is surgery. In some patients with no or minimal symptoms of the hernia a so-called “watchful-waiting-strategy” can be an alternative treatment approach. In some patients the surgical intervention can be prevented although in many patients a subsequent operation of the hernia will be necessary due to increasing hernia size or symptoms during “watchful-waiting”.
Modern surgical techniques in hernia surgery include the implantation of synthetic mesh (polypropylene mesh or other materials) to minimize the risk of recurrent hernia. If the patient refuses mesh implantation, a natural-tissue hernia repair (e.g. Shouldice-Repair) can be discussed with the patient as an individualized treatment approach.
Surgical therapy of groin hernias
For the treatment of groin or inguinal hernias, two main different surgical techniques can be offered to the patients: the “classical” open surgical technique (Lichtenstein-Repair) or the minimally-invasive laparo-endoscopic technique (TAPP, trans-abdominal preperitoneal plasty). In both techniques, the posterior wall of the inguinal canal is reinforced with synthetic mesh. Both techniques have proven their efficacy in the treatment of inguinal hernias. The techniques are equal with regard to the (very low) incidence of recurrent hernia, while a slight advantage exists for the laparo-endoscopic techniques with regard to postoperative pain. We prefer the laparo-endoscopic TAPP-repair in most suitable patients, while in some patients (e.g. recurrent hernia, large-scrotal hernia) a tailored-approach has to be discussed with the patient to offer the best possible individual treatment.
Beside the routine treatment of groin hernia, as a university medical center, we can offer special expertise in the treatment of recurrent hernias and chronic pain after groin hernia surgery.
Surgical therapy of umbilical, epigastric an incisional hernia
Different techniques - individualized to the patient’s hernia (size, location) - exist for the treatment of incisional, epigastric and umbilical hernias. Very small ventral hernias can be treated with sutured repair. Starting with a hernia size of 1-2 cm, the reconstruction of the abdominal wall should be reinforced with a synthetic mesh to reduce the risk of a recurrent hernia. Up to a hernia size of ≤4 cm a so called PUMP-Repair (Preperitoneal umbilical mesh plasty) can be performed with the open preperitoneal implantation of a mesh. Alternatively, minimally-invasive technique can be discussed also for relatively small ventral hernia < 4 cm especially in obese patients.
Bigger hernias ≥4 cm are routinely treated with a so-called Rives-Stoppa-Sublay-Herniotomy. In very large ventral hernias (>10 cm diameter) this procedure can be combined with anterior (Ramirez component separation) or posterior component separation (transversus-abdominis-release/TAR) to achieve fascial closure with wide mesh overlap and therefore adequate reconstruction of the abdominal wall. In our clinical routine, ventral hernia ranging from 4-10 cm are treated with minimally-invasive eTEP (extended totally extraperitoneal plasty) Rives-Stoppa-Sublay-Herniotomy. We can also offer simultaneous minimally-invasive component separation techniques. Open surgery is only necessary in very large or complex hernias.
The intraperitoneal mesh position used in the IPOM-technique (Intraperitoneal Onlay Mesh-Repair) is associated with several postoperative and especially long-term risks (intraperitoneal adhesions, mechanical bowel obstruction, bowel fistula). Hence, we only use this technique in very rare exceptional cases in which the implantation of the synthetic mesh to the sublay-position is technically not possible.
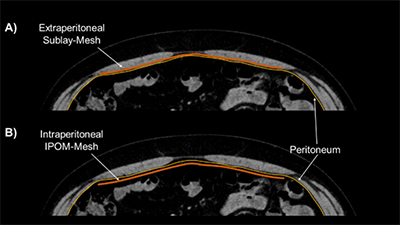
Fig.: Mesh-Positions in ventral hernia surgery
A) During a Sublay-Herniotomy, the synthetic mesh is implanted in the retromuscular space and therefore integrated into the abdominal wall. The synthetic mesh has no direct contact to the viscera, as the peritoneum and posterior rectus sheath is beneath the mesh and acts as a barrier towards the abdominal cavity. This mesh position can be achieved in the “classical” open Rives-Stoppa-Sublay-Herniotomy and in the minimally-invasive eTEP-Sublay-Technique.
B) Special coated IPOM-Composite Mesh are used for the IPOM-Technique (Intraperitoneal Onlay Mesh), as the synthetic mesh is implanted directly into the abdominal cavity in this technique.
Therapy of complex (recurrent) hernia
Very large ventral hernias (>15 cm) or hernias with a very large hernia sac-volume (>20% of the total peritoneal volume) often need additional surgical and/or preparatory measures, to accomplish successful and long-lasting closure of the hernia. With the above mentioned component separation techniques and in some cases combined with intraoperative fascial traction, a successful primary closure of the fascia can be achieved in most complex hernia cases. Additionally, in selected patients we do offer preparatory measures such as chemical component separation with botulinum toxin A-injection to the lateral abdominal wall muscles (in some cases combined with preoperative progressive pneumoperioneum). This intervention can improve the condition of the abdominal wall in selected patients with retracted fascial edges and therefore the conditions for successful closure of the fascia can be optimized preoperatively within 4-6 weeks prior to the surgery.
Obese patients are at risk for perioperative complications and recurrence of the treated hernias. We can therefore embed the management of the hernia in obese patients in a metabolic concept with preoperative weight-loss by nutrition counseling, the use of GLP-1-receptor agonists (e.g. Semaglutid®) or even in combination with prior metabolic surgery (sleeve-gastrectomy, Roux-en-Y gastric bypass) – which can be performed at our clinic as well. In these cases, we can offer an individual discussion to find the optimal treatment strategy for your individual case.